RPA implementation and OCR Reduced Healthcare Processing Time
INDUSTRY: Healthcare
Tags:
Overview
The national auto insurance company faced a significant challenge in processing a high volume of CMS 1500 medical claim forms manually, leading to extensive time consumption and elevated operational costs. RPA implementation could help to automate this process for improved accuracy, cost-efficiency, and enhanced control over the claims processing workflow.
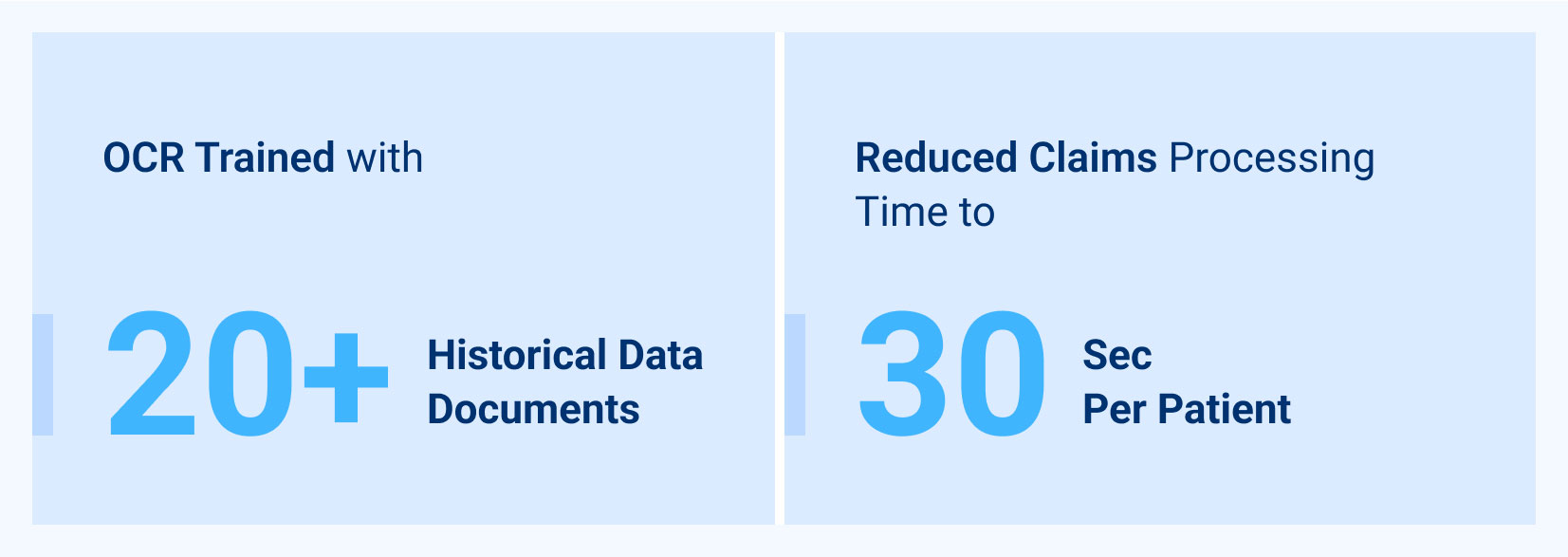
RPA automation rules were employed to achieve these goals. The process involved bot-driven tasks, including file retrieval, bill identification, OCR data extraction, block creation for data export, data validation, and secure data handling.
Successful RPA implementation with OCR reduced the processing time from hours to just 30 seconds per patient, while ensuring the utmost security of sensitive medical data through encryption and meticulous logging.
Challenges
The challenges faced by the national auto insurance company included:
- Manual Processing: Processing thousands of CMS 1500 medical claim forms manually was labor-intensive, time-consuming, and expensive.
- Error rate: Manual data entry posed a risk of inaccurate reimbursements, potentially leading to financial losses and customer dissatisfaction.
- Operational Costs: The extensive manual effort required for data entry incurred high operational costs requiring RPA implementation.
- Workflow Control: Lack of automation hindered control over the claims processing workflow.
- Data Security: Handling sensitive medical data necessitated robust security measures to prevent breaches and ensure compliance.
Solutions
After an RPA consulting with Accleirate, RPA implementation based on the principles of Industrial process automation was deployed and the following key solutions addressed the challenge.
- Speeding up of processes: Multiple bots were utilized to streamline the claims processing workflow, reducing manual intervention and speeding up processing.
- OCR Data Extraction: OCR technology was deployed to accurately extract and categorize data from CMS 1500 forms, improving data accuracy and consistency.
- Data Export and Validation: A structured approach was developed to export and validate data by matching extracted information to predefined blocks, ensuring data integrity and reducing errors.
- Data Security Measures: Implemented robust data security measures, including encryption at every step and comprehensive logging, to safeguard sensitive medical information and ensure compliance with data protection regulations.
Results
RPA Implementation and OCR technology yielded remarkable results:
- Processing Time Reduction: The time required to process medical claims was significantly reduced from hours to 30 seconds per patient.
- Cost Efficiency: Automation led to substantial cost savings by eliminating the need for extensive manual data entry.
- Accuracy: The risk of inaccurate reimbursements was minimized, enhancing overall accuracy in claims processing.
- Workflow Control: Automation provides greater control over the claims processing workflow, improving efficiency and reducing errors.
- Data Security: Sensitive medical data was safeguarded through encryption and comprehensive logging, ensuring compliance with data security standards and regulations.