Claim Management with Industrial Process Automation
INDUSTRY: Finance
Tags:
Overview
Claim management needs industrial process automation because it involves individuals or organizations requesting payment for losses, typically financial ones, from insurance companies or relevant entities. It encompasses various steps and offers significant benefits, including cost-saving, reduced processing time, improved accuracy, data analytics, enhanced customer satisfaction, and strategic advantages.

Challenges
- Complexity of Verification: The verification and approval process can be intricate, requiring thorough examination of claims to ensure their validity, needing RPA as a service.
- Manual Processing: Traditional, manual claim management can be time-consuming, costly, and prone to errors and discrepancies.
- Data Quality: Maintaining data accuracy and consistency can be challenging when multiple parties are involved in the claim process.
- Fraud Detection: Identifying fraudulent claims poses a significant challenge, as fraudsters continually evolve their tactics.
Solution
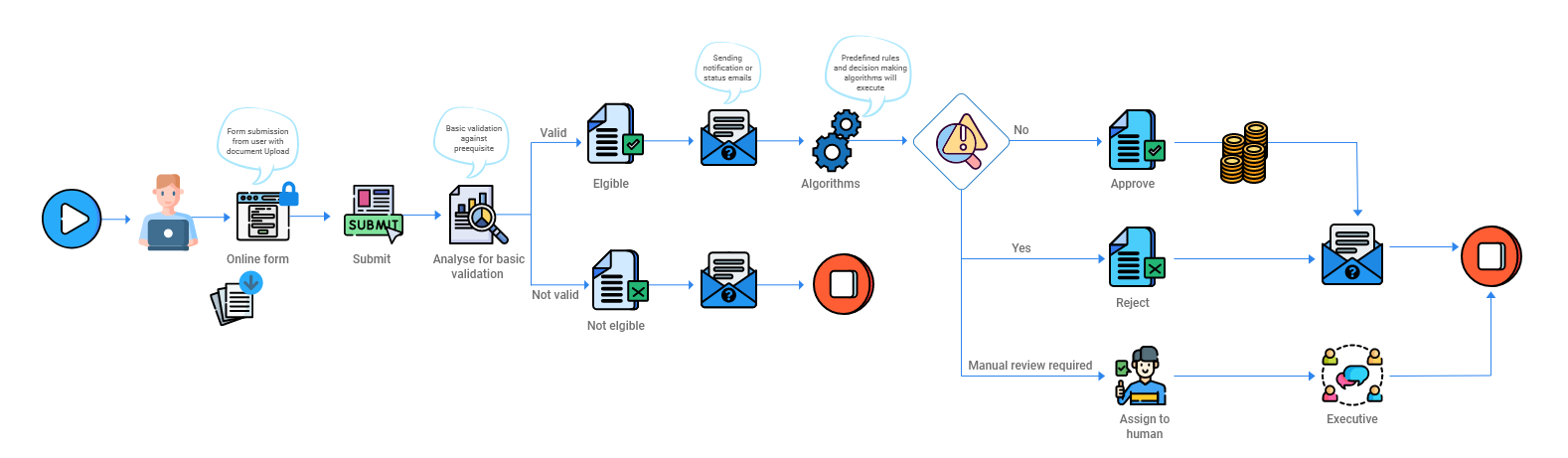
Accelirate’s RPA implementation addressed the bigger challenge and automated solutions for claim management:
- Cost Saving: Industrial process automation reduced labor costs and operational expenses, potentially saving up to 30% of overall costs.
- Reduced Downtime: Automated solutions expedited claim processing, saving up to 50% of the time required.
- Optimum Accuracy: Automation reduced errors, omissions, and discrepancies, enhancing data quality and reliability.
- Impactful Data Analytics: Automated systems enabled analysis of claim data, and identification of patterns, trends, and potential fraud which led to informed decision-making and strategic improvements.
- Enhanced Customer Satisfaction: Automation provides regular claim status updates, faster processing, and valuable resources and guidance through email, resulting in improved customer satisfaction.
Expected Benefits
- Cost saving: Saving labor costs and operational expense automation solutions can potentially help the organization to save up to 30% of its overall costs.
- Reduced downtime: The automated solution can save up to 50% of the time required for claim processing, which could save a thousand hours per year.
- Optimum accuracy: The solution will reduce errors, omissions, and discrepancies owing to fewer human interventions and improve quality.
- Impactful data analytics: Our client organization will be able to identify patterns, trends, and fraud and explore opportunities that can eventually help in better decision-making and strategic growth improvements.
- Enhanced customer satisfaction: Regular updates about the claim status, faster processing, and useful resources & guidance offered via email can significantly improve customer satisfaction
Results
- Customer Retention: Improved customer satisfaction and loyalty boosted retention, attracting new customers.
- Fraud Detection/Risk Management: Proactive fraud detection and risk management ensure long-term sustainability; this case is also sometimes seen in Hyperautomation in banking.
- Competitive Differentiation: Cost-saving, data analytics, faster processing, and customer satisfaction set organizations apart.
- Regulatory Compliance: Automation helps meet regulatory requirements, avoiding fines and penalties.